(N. Trigeminus; Fifth Or Trifacial Nerve)
The trigeminal nerve is the largest cranial nerve and is the great sensory nerve of the head and face, and the motor nerve of the muscles of mastication. | 1 |
| It emerges from the side of the pons, near its upper border, by a small motor and a large sensory root—the former being situated in front of and medial to the latter. | 2 |
| |
| Motor Root.—The fibers of the motor root arise from two nuclei, a superior and an inferior. The superior nucleus consists of a strand of cells occupying the whole length of the lateral portion of the gray substance of the cerebral aqueduct. The inferior or chief nucleus is situated in the upper part of the pons, close to its dorsal surface, and along the line of the lateral margin of the rhomboid fossa. The fibers from the superior nucleus constitute the mesencephalic root: they descend through the mid-brain, and, entering the pons, join with the fibers from the lower nucleus, and the motor root, thus formed, passes forward through the pons to its point of emergence. It is uncertain whether the mesencephalic root is motor or sensory. | 3 |
| |
| Sensory Root.—The fibers of the sensory root arise from the cells of the semilunar ganglion which lies in a cavity of the dura mater near the apex of the petrous part of the temporal bone. They pass backward below the superior petrosal sinus and tentorium cerebelli, and, entering the pons, divide into upper and lower roots. The upper root ends partly in a nucleus which is situated in the pons lateral to the lower motor nucleus, and partly in the locus cæruleus; the lower root descends through the pons and medulla oblongata, and ends in the upper part of the substantia gelatinosa of Rolando. This lower root is sometimes named the spinal root of the nerve. Medullation of the fibers of the sensory root begins about the fifth month of fetal life, but the whole of its fibers are not medullated until the third month after birth. | 4 |
| The Semilunar Ganglion (ganglion semilunare [Gasseri]; Gasserian ganglion) occupies a cavity (cavum Meckelii) in the dura mater covering the trigeminal impression near the apex of the petrous part of the temporal bone. It is somewhat crescentic in shape, with its convexity directed forward: medially, it is in relation with the internal carotid artery and the posterior part of the cavernous sinus. The motor root runs in front of and medial to the sensory root, and passes beneath the ganglion; it leaves the skull through the foramen ovale, and, immediately below this foramen, joins the mandibular nerve. The greater superficial petrosal nerve lies also underneath the ganglion. | 5 |
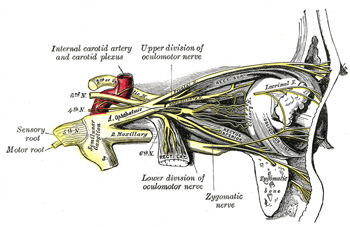
| The ganglion receives, on its medial side, filaments from the carotid plexus of the sympathetic. It give off minute branches to the tentorium cerebelli, and to the dura mater in the middle fossa of the cranium. From its convex border, which is directed forward and lateralward, three large nerves proceed, viz., the ophthalmic, maxillary, and mandibular. The ophthalmic and maxillary consist exclusively of sensory fibers; the mandibular is joined outside the cranium by the motor root. | 6 |
| Associated with the three divisions of the trigeminal nerve are four small ganglia. The ciliary ganglion is connected with the ophthalmic nerve; the sphenopalatine ganglion with the maxillary nerve; and the otic and submaxillary ganglia with the mandibular nerve. All four receive sensory filaments from the trigeminal, and motor and sympathetic filaments from various sources; these filaments are called the roots of the ganglia. | 7 |
| The Ophthalmic Nerve (n. ophthalmicus) (Figs. 776, 777), or first division of the trigeminal, is a sensory nerve. It supplies branches to the cornea, ciliary body, and iris; to the lacrimal gland and conjunctiva; to the part of the mucous membrane of the nasal cavity; and to the skin of the eyelids, eyebrow, forehead, and nose. It is the smallest of the three divisions of the trigeminal, and arises from the upper part of the semilunar ganglion as a short, flattened band, about 2.5 cm. long, which passes forward along the lateral wall of the cavernous sinus, below the oculomotor and trochlear nerves; just before entering the orbit, through the superior orbital fissure, it divides into three branches, lacrimal, frontal, and nasociliary. | 8 |
| The ophthalmic nerve is joined by filaments from the cavernous plexus of the sympathetic, and communicates with the oculomotor, trochlear, and abducent nerves; it gives off a recurrent filament which passes between the layers of the tentorium. | 9 |
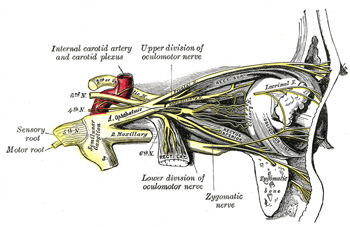 |
FIG. 777– Nerves of the orbit, and the ciliary ganglion. Side view. (See enlarged image) |
| |
| The Lacrimal Nerve (n. lacrimalis) is the smallest of the three branches of the ophthalmic. It sometimes receives a filament from the trochlear nerve, but this is possibly derived from the branch which goes from the ophthalmic to the trochlear nerve. It passes forward in a separate tube of dura mater, and enters the orbit through the narrowest part of the superior orbital fissure. In the orbit it runs along the upper border of the Rectus lateralis, with the lacrimal artery, and communicates with the zygomatic branch of the maxillary nerve. It enters the lacrimal gland and gives off several filaments, which supply the gland and the conjunctiva. Finally it pierces the orbital septum, and ends in the skin of the upper eyelid, joining with filaments of the facial nerve. The lacrimal nerve is occasionally absent, and its place is then taken by the zygomaticotemporal branch of the maxillary. Sometimes the latter branch is absent, and a continuation of the lacrimal is substituted for it. | 10 |
| The Frontal Nerve (n. frontalis) is the largest branch of the ophthalmic, and may be regarded, both from its size and direction, as the continuation of the nerve. It enters the orbit through the superior orbital fissure, and runs forward between the Levator palpebræ superioris and the periosteum. Midway between the apex and base of the orbit it divides into two branches, supratrochlear and supraorbital. | 11 |
| The supratrochlear nerve (n. supratrochlearis), the smaller of the two, passes above the pulley of the Obliquus superior, and gives off a descending filament, to join the infratrochlear branch of the nasociliary nerve. It then escapes from the orbit between the pulley of the Obliquus superior and the supraorbital foramen, curves up on to the forehead close to the bone, ascends beneath the Corrugator and Frontalis, and dividing into branches which pierce these muscles, it supplies the skin of the lower part of the forehead close to the middle line and sends filaments to the conjunctiva and skin of the upper eyelid. | 12 |
| The supraorbital nerve (n. supraorbitalis) passes through the supraorbital foramen, and gives off, in this situation, palpebral filaments to the upper eyelid. It then ascends upon the forehead, and ends in two branches, a medial and a lateral, which supply the integument of the scalp, reaching nearly as far back as the lambdoidal suture; they are at first situated beneath the Frontalis, the medial branch perforating the muscle, the lateral branch the galea aponeurotica. Both branches supply small twigs to the pericranium. | 13 |
| The Nasociliary Nerve (n. nasociliaris; nasal nerve) is intermediate in size between the frontal and lacrimal, and is more deeply placed. It enters the orbit between the two heads of the Rectus lateralis, and between the superior and inferior rami of the oculomotor nerve. It passes across the optic nerve and runs obliquely beneath the Rectus superior and Obliquus superior, to the medial wall of the orbital cavity. Here it passes through the anterior ethmoidal foramen, and, entering the cavity of the cranium, traverses a shallow groove on the lateral margin of the front part of the cribriform plate of the ethmoid bone, and runs down, through a slit at the side of the crista galli, into the nasal cavity. It supplies internal nasal branches to the mucous membrane of the front part of the septum and lateral wall of the nasal cavity. Finally, it emerges, as the external nasal branch, between the lower border of the nasal bone and the lateral nasal cartilage, and, passing down beneath the Nasalis muscle, supplies the skin of the ala and apex of the nose. | 14 |
| The nasociliary nerve gives off the following branches, viz.: the long root of the ciliary ganglion, the long ciliary, and the ethmoidal nerves. | 15 |
| The long root of the ciliary ganglion (radix longa ganglii ciliaris) usually arises from the nasociliary between the two heads of the Rectus lateralis. It passes forward on the lateral side of the optic nerve, and enters the postero-superior angle of the ciliary ganglion; it is sometimes joined by a filament from the cavernous plexus of the sympathetic, or from the superior ramus of the trochlear nerve. | 16 |
| The long ciliary nerves (nn. ciliares longi), two or three in number, are given off from the nasociliary, as it crosses the optic nerve. They accompany the short ciliary nerves from the ciliary ganglion, pierce the posterior part of the sclera, and running forward between it and the choroid, are distributed to the iris and cornea. The long ciliary nerves are supposed to contain sympathetic fibers from the superior cervical ganglion to the Dilator pupillæ muscle. | 17 |
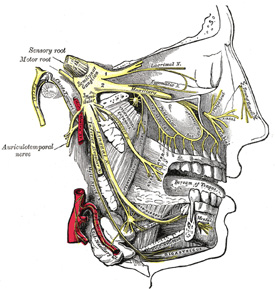
| The infratrochlear nerve (n. infratrochlearis) is given off from the nasociliary just before it enters the anterior ethmoidal foramen. It runs forward along the upper border of the Rectus medialis, and is joined, near the pulley of the Obliquus superior, by a filament from the supratrochlear nerve. It then passes to the medial angle of the eye, and supplies the skin of the eyelids and side of the nose, the conjunctiva, lacrimal sac, and caruncula lacrimalis. | 18 |
| The ethmoidal branches (nn. ethmoidales) supply the ethmoidal cells; the posterior branch leaves the orbital cavity through the posterior ethmoidal foramen and gives some filaments to the sphenoidal sinus. | 19 |
| |
| The Ciliary Ganglion (ophthalmic or lenticular ganglion) (Figs. 775, 777).—The ciliary ganglion is a small, sympathetic ganglion, of a reddish-gray color, and about the size of a pin’s head; it is situated at the back part of the orbit, in some loose fat between the optic nerve and the Rectus lateralis muscle, lying generally on the lateral side of the ophthalmic artery. | 20 |
| Its roots are three in number, and enter its posterior border. One, the long or sensory root, is derived from the nasociliary nerve, and joins its postero-superior angle. The second, the short or motor root, is a thick nerve (occasionally divided into two parts) derived from the branch of the oculomotor nerve to the Obliquus inferior, and connected with the postero-inferior angle of the ganglion. The motor root is supposed to contain sympathetic efferent fibers (preganglionic fibers) from the nucleus of the third nerve in the mid-brain to the ciliary ganglion where they form synapses with neurons whose fibers (postganglionic) pass to the Ciliary muscle and to Sphincter muscle of the pupil. The third, the sympathetic root, is a slender filament from the cavernous plexus of the sympathetic; it is frequently blended with the long root. According to Tiedemann, the ciliary ganglion receives a twig of communication from the sphenopalatine ganglion. | 21 |
| Its branches are the short ciliary nerves. These are delicate filaments, from six to ten in number, which arise from the forepart of the ganglion in two bundles connected with its superior and inferior angles; the lower bundle is the larger. They run forward with the ciliary arteries in a wavy course, one set above and the other below the optic nerve, and are accompanied by the long ciliary nerves from the nasociliary. They pierce the sclera at the back part of the bulb of the eye, pass forward in delicate grooves on the inner surface of the sclera, and are distributed to the Ciliaris muscle, iris, and cornea. Tiedemann has described a small branch as penetrating the optic nerve with the arteria centralis retinæ. | 22 |
| The Maxillary Nerve (n. maxillaris; superior maxillary nerve) (Fig. 778), or second division of the trigeminal, is a sensory nerve. It is intermediate, both in position and size, between the ophthalmic and mandibular. It begins at the middle of the semilunar ganglion as a flattened plexiform band, and, passing horizontally forward, it leaves the skull through the foramen rotundum, where it becomes more cylindrical in form, and firmer in texture. It then crosses the pterygopalatine fossa, inclines lateralward on the back of the maxilla, and enters the orbit through the inferior orbital fissure; it traverses the infraorbital groove and canal in the floor of the orbit, and appears upon the face at the infraorbital foramen. 131 At its termination, the nerve lies beneath the Quadratus labii superioris, and divides into a leash of branches which spread out upon the side of the nose, the lower eyelid, and the upper lip, joining with filaments of the facial nerve. | 23 |
| |
| Branches.—Its branches may be divided into four groups, according as they are given off in the cranium, in the pterygopalatine fossa, in the infraorbital canal, or on the face. | 24 |
| In the Cranium…………… |
Middle meningeal. |
|
| In the Pterygopalatine Fossa… |
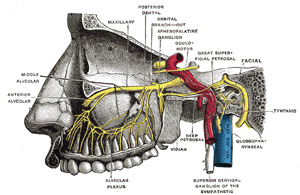
Zygomatic. |
| Sphenopalatine. |
| Posterior superior alveolar. |
|
| In the Infraorbital Canal……… |
Anterior superior alveolar. |
| Middle superior alveolar. |
|
| On the Face………………… |
Inferior palpebral. |
| External nasal. |
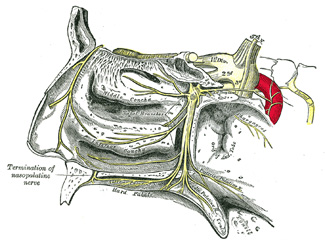
| Superior labial. |
|
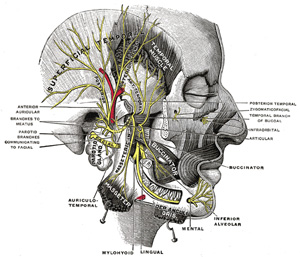
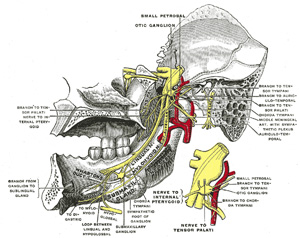
| The Middle Meningeal Nerve (n. meningeus medius; meningeal or dural branch) is given off from the maxillary nerve directly after its origin from the semilunar ganglion; it accompanies the middle meningeal artery and supplies the dura mater. | 25 |
| The Zygomatic Nerve (n. zygomaticus; temporomalar nerve; orbital nerve) arises in the pterygopalatine fossa, enters the orbit by the inferior orbital fissure, and divides at the back of that cavity into two branches, zygomaticotemporal and zygomaticofacial. | 26 |
| The zygomaticotemporal branch (ramus zygomaticotemporalis; temporal branch) runs along the lateral wall of the orbit in a groove in the zygomatic bone, receives a branch of communication from the lacrimal, and, passing through a foramen in the zygomatic bone, enters the temporal fossa. It ascends between the bone, and substance of the Temporalis muscle, pierces the temporal fascia about 2.5 cm. above the zygomatic arch, and is distributed to the skin of the side of the forehead, and communicates with the facial nerve and with the aurićulotemporal branch of the mandibular nerve. As it pierces the temporal fascia, it gives off a slender twig, which runs between the two layers of the fascia to the lateral angle of the orbit. | 27 |
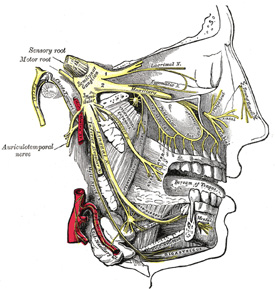 |
FIG. 778– Distribution of the maxillary and mandibular nerves, and the submaxillary ganglion. (See enlarged image) |
| |
| The zygomaticofacial branch (ramus zygomaticofacialis; malar branch) passes along the infero-lateral angle of the orbit, emerges upon the face through a foramen in the zygomatic bone, and, perforating the Orbicularis oculi, supplies the skin on the prominence of the cheek. It joins with the facial nerve and with the inferior palpebral branches of the maxillary. | 28 |
| The Sphenopalatine Branches (nn. sphenopalatini), two in number, descend to the sphenopalatine ganglion. | 29 |
| The Posterior Superior Alveolar Branches (rami alveolares superiores posteriores; posterior superior dental branches) arise from the trunk of the nerve just before it enters the infraorbital groove; they are generally two in number, but sometimes arise by a single trunk. They descend on the tuberosity of the maxilla and give off several twigs to the gums and neighboring parts of the mucous membrane of the cheek. They then enter the posterior alveolar canals on the infratemporal surface of the maxilla, and, passing from behind forward in the substance of the bone, communicate with the middle superior alveolar nerve, and give off branches to the lining membrane of the maxillary sinus and three twigs to each molar tooth; these twigs enter the foramina at the apices of the roots of the teeth. | 30 |
| The Middle Superior Alveolar Branch (ramus alveolaris superior medius; middle superior dental branch), is given off from the nerve in the posterior part of the infraorbital canal, and runs downward and forward in a canal in the lateral wall of the maxillary sinus to supply the two premolar teeth. It forms a superior dental plexus with the anterior and posterior superior alveolar branches. | 31 |
| The Anterior Superior Alveolar Branch (ramus alveolaris superior anteriores; anterior superior dental branch), of considerable size, is given off from the nerve just before its exit from the infraorbital foramen; it descends in a canal in the anterior wall of the maxillary sinus, and divides into branches which supply the incisor and canine teeth. It communicates with the middle superior alveolar branch, and gives off a nasal branch, which passes through a minute canal in the lateral wall of the inferior meatus, and supplies the mucous membrane of the anterior part of the inferior meatus and the floor of the nasal cavity, communicating with the nasal branches from the sphenopalatine ganglion. | 32 |
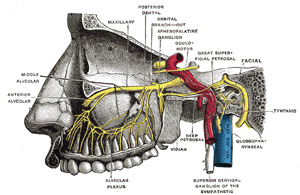 |
FIG. 779– Alveolar branches of superior maxillary nerve and sphenopalatine ganglion. (Testut.) (See enlarged image) |
| |
| The Inferior Palpebral Branches (rami palpebrales inferiores; palpebral branches) ascend behind the Orbicularis oculi. They supply the skin and conjunctiva of the lower eyelid, joining at the lateral angle of the orbit with the facial and zygomaticofacial nerves. | 33 |
| The External Nasal Branches (rami nasales externi) supply the skin of the side of the nose and of the septum mobile nasi, and join with the terminal twigs of the nasociliary nerve. | 34 |
| The Superior Labial Branches (rami labiales superiores; labial branches), the largest and most numerous, descend behind the Quadratus labii superioris, and are distributed to the skin of the upper lip, the mucous membrane of the mouth, and labial glands. They are joined, immediately beneath the orbit, by filaments from the facial nerve, forming with them the infraorbital plexus. | 35 |
| |
| Sphenopalatine Ganglion (ganglion of Meckel) (Fig. 780).—The sphenopalatine ganglion, the largest of the sympathetic ganglia associated with the branches of the trigeminal nerve, is deeply placed in the pterygopalatine fossa, close to the sphenopalatine foramen. It is triangular or heart-shaped, of a reddish-gray color, and is situated just below the maxillary nerve as it crosses the fossa. It receives a sensory, a motor, and a sympathetic root. | 36 |
| Its sensory root is derived from two sphenopalatine branches of the maxillary nerve; their fibers, for the most part, pass directly into the palatine nerves; a few, however, enter the ganglion, constituting its sensory root. Its motor root is probably derived from the nervus intermedius through the greater superficial petrosal nerve and is supposed to consist in part of sympathetic efferent (preganglionic) fibers from the medulla. In the sphenopalatine ganglion they form synapses with neurons whose postganglionic axons, vasodilator and secretory fibers, are distributed with the deep branches of the trigeminal to the mucous membrane of the nose, soft palate, tonsils, uvula, roof of the mouth, upper lip and gums, and to the upper part of the pharynx. Its sympathetic root is derived from the carotid plexus through the deep petrosal nerve. These two nerves join to form the nerve of the pterygoid canal before their entrance into the ganglion. | 37 |
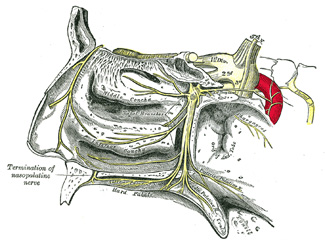 |
FIG. 780– The sphenopalatine ganglion and its branches. (See enlarged image) |
| |
| The greater superficial petrosal nerve (n. petrosus superficialis major; large superficial petrosal nerve) is given off from the genicular ganglion of the facial nerve; it passes through the hiatus of the facial canal, enters the cranial cavity, and runs forward beneath the dura mater in a groove on the anterior surface of the petrous portion of the temporal bone. It then enters the cartilaginous substance which fills the foramen lacerum, and joining with the deep petrosal branch forms the nerve of the pterygoid canal. | 38 |
| The deep petrosal nerve (n. petrosus profundus; large deep petrosal nerve) is given off from the carotid plexus, and runs through the carotid canal lateral to the internal carotid artery. It then enters the cartilaginous substance which fills the foramen lacerum, and joins with the greater superficial petrosal nerve to form the nerve of the pterygoid canal. | 39 |
| The nerve of the pterygoid canal (n. canalis pterygoidei [Vidii]; Vidian nerve), formed by the junction of the two preceding nerves in the cartilaginous substance which fills the foramen lacerum, passes forward, through the pterygoid canal, with the corresponding artery, and is joined by a small ascending sphenoidal branch from the otic ganglion. Finally, it enters the pterygopalatine fossa, and joins the posterior angle of the sphenopalatine ganglion. | 40 |
| |
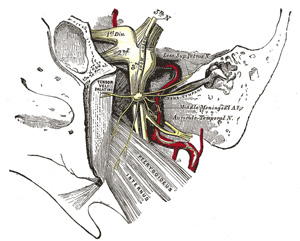
| Branches of Distribution.—These are divisible into four groups, viz., orbital, palatine, posterior superior nasal, and pharyngeal. | 41 |
| The orbital branches (rami orbitales; ascending branches) are two or three delicate filaments, which enter the orbit by the inferior orbital fissure, and supply the periosteum. According to Luschka, some filaments pass through foramina in the frontoethmoidal suture to supply the mucous membrane of the posterior ethmoidal and sphenoidal sinuses. | 42 |
| The palatine nerves (nn. palatini; descending branches) are distributed to the roof of the mouth, soft palate, tonsil, and lining membrane of the nasal cavity. Most of their fibers are derived from the sphenopalatine branches of the maxillary nerve. They are three in number: anterior, middle, and posterior. | 43 |
| The anterior palatine nerve (n. palatinus anterior) descends through the pterygopalatine canal, emerges upon the hard palate through the greater palatine foramen, and passes forward in a groove in the hard palate, nearly as far as the incisor teeth. It supplies the gums, the mucous membrane and glands of the hard palate, and communicates in front with the terminal filaments of the nasopalatine nerve. While in the pterygopalatine canal, it gives off posterior inferior nasal branches, which enter the nasal cavity through openings in the palatine bone, and ramify over the inferior nasal concha and middle and inferior meatuses; at its exit from the canal, a palatine branch is distributed to both surfaces of the soft palate. | 44 |
| The middle palatine nerve (n. palatinus medius) emerges through one of the minor palatine canals and distributes branches to the uvula, tonsil, and soft palate. It is occasionally wanting. | 45 |
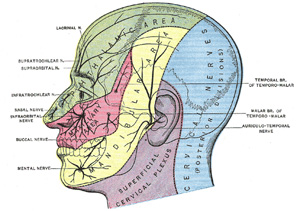
| The posterior palatine nerve (n. palatinus posterior) descends through the pterygopalatine canal, and emerges by a separate opening behind the greater palatine foramen; it supplies the soft palate, tonsil, and uvula. The middle and posterior palatine join with the tonsillar branches of the glossopharyngeal to form a plexus (circulus tonsillaris) around the tonsil. | 46 |
| The posterior superior nasal branches (rami nasales posteriores superiores) are distributed to the septum and lateral wall of the nasal fossa. They enter the posterior part of the nasal cavity by the sphenopalatine foramen and supply the mucous membrane covering the superior and middle nasal conchæ, the lining of the posterior ethmoidal cells, and the posterior part of the septum. One branch, longer and larger than the others, is named the nasopalatine nerve. It enters the nasal cavity through the sphenopalatine foramen, passes across the roof of the nasal cavity below the orifice of the sphenoidal sinus to reach the septum, and then runs obliquely downward and forward between the periosteum and mucous membrane of the lower part of the septum. It descends to the roof of the mouth through the incisive canal and communicates with the corresponding nerve of the opposite side and with the anterior palatine nerve. It furnishes a few filaments to the mucous membrane of the nasal septum. | 47 |
| The pharyngeal nerve (pterygopalatine nerve) is a small branch arising from the posterior part of the ganglion. It passes through the pharyngeal canal with the pharyngeal branch of the internal maxillary artery, and is distributed to the mucous membrane of the nasal part of the pharynx, behind the auditory tube. | 48 |
| The mandibular nerve (n. mandibularis; inferior maxillary nerve) (Figs. 778, 781) supplies the teeth and gums of the mandible, the skin of the temporal region, the auricula, the lower lip, the lower part of the face, and the muscles of mastication; it also supplies the mucous membrane of the anterior two-thirds of the tongue. It is the largest of the three divisions of the fifth, and is made up of two roots: a large, sensory root proceeding from the inferior angle of the semilunar ganglion, and a small motor root (the motor part of the trigeminal), which passes beneath the ganglion, and unites with the sensory root, just after its exit through the foramen ovale. Immediately beneath the base of the skull, the nerve gives off from its medial side a recurrent branch (nervus spinosus) and the nerve to the Pterygoideus internus, and then divides into two trunks, an anterior and a posterior. | 49 |
| The Nervus Spinosus (recurrent or meningeal branch) enters the skull through the foramen spinosum with the middle meningeal artery. It divides into two branches, anterior and posterior, which accompany the main divisions of the artery and supply the dura mater; the posterior branch also supplies the mucous lining of the mastoid cells; the anterior communicates with the meningeal branch of the maxillary nerve. | 50 |
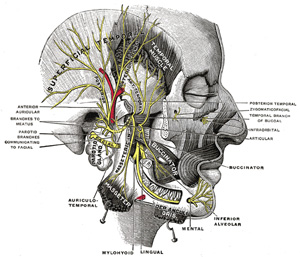 |
FIG. 781– Mandibular division of the trifacial nerve. (Testut.) (See enlarged image) |
| |
| |
| The Internal Pterygoid Nerve (n. pterygoideus internus).—The nerve to the Pterygoideus internus is a slender branch, which enters the deep surface of the muscle; it gives off one or two filaments to the otic ganglion. | 51 |
| The anterior and smaller division of the mandibular nerve receives nearly the whole of the fibers of the motor root of the nerve, and supplies the muscles of mastication and the skin and mucous membrane of the cheek. Its branches are the masseteric, deep temporal, buccinator, and external pterygoid. | 52 |
| The Masseteric Nerve (n. massetericus) passes lateralward, above the Pterygoideus externus, in front of the temporomandibular articulation, and behind the tendon of the Temporalis; it crosses the mandibular notch with the masseteric artery, to the deep surface of the Masseter, in which it ramifies nearly as far as its anterior border. It gives a filament to the temporomandibular joint. | 53 |
| The Deep Temporal Nerves (nn. temporales profundi) are two in number, anterior and posterior. They pass above the upper border of the Pterygoideus externus and enter the deep surface of the Temporalis. The posterior branch, of small size, is placed at the back of the temporal fossa, and sometimes arises in common with the masseteric nerve. The anterior branch is frequently given off from the buccinator nerve, and then turns upward over the upper head of the Pterygoideus externus. Frequently a third or intermediate branch is present. | 54 |
| The Buccinator Nerve (n. buccinatorus; long buccal nerve) passes forward between the two heads of the Pterygoideus externus, and downward beneath or through the lower part of the Temporalis; it emerges from under the anterior border of the Masseter, ramifies on the surface of the Buccinator, and unites with the buccal branches of the facial nerve. It supplies a branch to the Pterygoideus externus during its passage through that muscle, and may give off the anterior deep temporal nerve. The buccinator nerve supplies the skin over the Buccinator, and the mucous membrane lining its inner surface. | 55 |
| |
| External Pterygoid Nerve (n. pterygoideus externus).—The nerve to the Pterygoideus externus frequently arises in conjunction with the buccinator nerve, but it may be given off separately from the anterior division of the mandibular nerve. It enters the deep surface of the muscle. | 56 |
| The posterior and larger division of the mandibular nerve is for the most part sensory, but receives a few filaments from the motor root. It divides into auriculotemporal, lingual, and inferior alveolar nerves. | 57 |
| The Auriculotemporal Nerve (n. auriculotemporalis) generally arises by two roots, between which the middle meningeal artery ascends. It runs backward beneath the Pterygoideus externus to the medial side of the neck of the mandible. It then turns upward with the superficial temporal artery, between the auricula and condyle of the mandible, under cover of the parotid gland; escaping from beneath the gland, it ascends over the zygomatic arch, and divides into superficial temporal branches. | 58 |
| The branches of communication of the auriculotemporal nerve are with the facial nerve and with the otic ganglion. The branches to the facial, usually two in number, pass forward from behind the neck of the mandible and join the facial nerve at the posterior border of the Masseter. The filaments to the otic ganglion are derived from the roots of the auriculotemporal nerve close to their origin. | 59 |
| Its branches of distribution are: | 60 |
| Anterior auricular. |
|
Articular. |
| Branches to the external acoustic meatus. |
|
Parotid. |
| Superficial temporal. |
|
| The anterior auricular branches (nn. auriculares anteriores) are usually two in number; they supply the front of the upper part of the auricula, being distributed principally to the skin covering the front of the helix and tragus. | 61 |
| The branches to the external acoustic meatus (n. meatus auditorii externi), two in number, enter the meatus between its bony and cartilaginous portions and supply the skin lining it; the upper one sends a filament to the tympanic membrane. | 62 |
| The articular branches consist of one or two twigs which enter the posterior part of the temporomandibular joint. | 63 |
| The parotid branches (rami parotidei) supply the parotid gland. | 64 |
| The superficial temporal branches (rami temporales superficiales) accompany the superficial temporal artery to the vertex of the skull; they supply the skin of the temporal region and communicate with the facial and zygomaticotemporal nerves. | 65 |
| The Lingual Nerve (n. lingualis) supplies the mucous membrane of the anterior two-thirds of the tongue. It lies at first beneath the Pterygoideus externus, medial to and in front of the inferior alveolar nerve, and is occasionally joined to this nerve by a branch which may cross the internal maxillary artery. The chorda tympani also joins it at an acute angle in this situation. The nerve then passes between the Pterygoideus internus and the ramus of the mandible, and crosses obliquely to the side of the tongue over the Constrictor pharyngis superior and Styloglossus, and then between the Hyoglossus and deep part of the submaxillary gland; it finally runs across the duct of the submaxillary gland, and along the tongue to its tip, lying immediately beneath the mucous membrane. | 66 |
| Its branches of communication are with the facial (through the chorda tympani), the inferior alveolar and hypoglossal nerves, and the submaxillary ganglion. The branches to the submaxillary ganglion are two or three in number; those connected with the hypoglossal nerve form a plexus at the anterior margin of the Hyoglossus. | 67 |
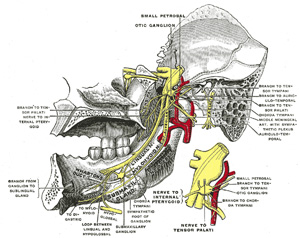 |
FIG. 782– Mandibular division of trifacial nerve, seen from the middle line. The small figure is an enlarged view of the otic ganglion. (Testut.) (See enlarged image) |
| |
| Its branches of distribution supply the sublingual gland, the mucous membrane of the mouth, the gums, and the mucous membrane of the anterior two-thirds of the tongue; the terminal filaments communicate, at the tip of the tongue, with the hypoglossal nerve. | 68 |
| The Inferior Alveolar Nerve (n. alveolaris inferior; inferior dental nerve)(Fig. 782) is the largest branch of the mandibular nerve. It descends with the inferior alveolar artery, at first beneath the Pterygoideus externus, and then between the sphenomandibular ligament and the ramus of the mandible to the mandibular foramen. It then passes forward in the mandibular canal, beneath the teeth, as far as the mental foramen, where it divides into two terminal branches, incisive and mental. | 69 |
| The branches of the inferior alveolar nerve are the mylohyoid, dental, incisive, and mental. | 70 |
| The mylohyoid nerve (n. mylohyoideus) is derived from the inferior alveolar just before it enters the mandibular foramen. It descends in a groove on the deep surface of the ramus of the mandible, and reaching the under surface of the Mylohyoideus supplies this muscle and the anterior belly of the Digastricus. | 71 |
| The dental branches supply the molar and premolar teeth. They correspond in number to the roots of those teeth; each nerve entering the orifice at the point of the root, and supplying the pulp of the tooth; above the alveolar nerve they form an inferior dental plexus. | 72 |
| The incisive branch is continued onward within the bone, and supplies the canine and incisor teeth. | 73 |
| The mental nerve (n. mentalis) emerges at the mental foramen, and divides beneath the Triangularis muscle into three branches; one descends to the skin of the chin, and two ascend to the skin and mucous membrane of the lower lip; these branches communicate freely with the facial nerve. | 74 |
| Two small ganglia, the otic and the submaxillary, are connected with the mandibular nerve. | 75 |
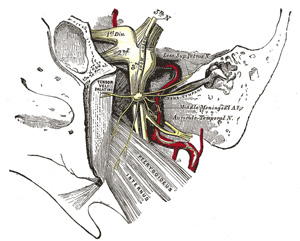 |
FIG. 783– The otic ganglion and its branches. (See enlarged image) |
| |
| |
| Otic Ganglion (ganglion oticum)(Fig. 783).—The otic ganglion is a small, ovalshaped, flattened ganglion of a reddish-gray color, situated immediately below the foramen ovale; it lies on the medial surface of the mandibular nerve, and surrounds the origin of the nerve to the Pterygoideus internus. It is in relation, laterally, with the trunk of the mandibular nerve at the point where the motor and sensory roots join; medially, with the cartilaginous part of the auditory tube, and the origin of the Tensor veli palatini; posteriorly, with the middle meningeal artery. | 76 |
| |
| Branches of Communication.—It is connected by two or three short filaments with the nerve to the Pterygoideus internus, from which it may obtain a motor, and possibly a sensory root. It communicates with the glossopharyngeal and facial nerves, through the lesser superficial petrosal nerve continued from the tympanic plexus, and through this nerve it probably receives a root from the glossopharyngeal and a motor root from the facial; its sympathetic root consists of a filament from the plexus surrounding the middle meningeal artery. The fibers from the glossopharyngeal which pass to the otic ganglion in the small superficial petrosal are supposed to be sympathetic efferent (preganglionic) fibers from the dorsal nucleus or inferior salivatory nucleus of the medulla. Fibers (postganglionic) from the otic ganglion with which these form synapses are supposed to pass with the auriculotemporal nerve to the parotid gland. A slender filament (sphenoidal) ascends from it to the nerve of the Pterygoid canal, and a small branch connects it with the chorda tympani. | 77 |
| Its branches of distribution are: a filament to the Tensor tympani, and one to the Tensor veli palatini. The former passes backward, lateral to the auditory tube; the latter arises from the ganglion, near the origin of the nerve to the Pterygoideus internus, and is directed forward. The fibers of these nerves are, however, mainly derived from the nerve to the Pterygoideus internus. | 78 |
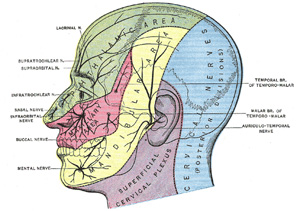 |
FIG. 784– Sensory areas of the head, showing the general distribution of the three divisions of the fifth nerve. (Modified from Testut.) (See enlarged image) |
| |
| |
| Submaxillary Ganglion (ganglion submaxillare)(Fig. 778).—The submaxillary ganglion is of small size and is fusiform in shape. It is situated above the deep portion of the submaxillary gland, on the hyoglossus, near the posterior border of the Mylohyoideus, and is connected by filaments with the lower border of the lingual nerve. It is suspended from the lingual nerve by two filaments which join the anterior and posterior parts of the ganglion. Through the posterior of these it receives a branch from the chorda tympani nerve which runs in the sheath of the lingual; these are sympathetic efferent (preganglionic) fibers from the facial nucleus or the superior salivatory nucleus of the medulla oblongata that terminate in the submaxillary ganglion. The postganglionic fibers pass to the submaxillary gland, it communicates with the sympathetic by filaments from the sympathetic plexus around the external maxillary artery. | 79 |
| Its branches of distribution are five or six in number; they arise from the lower part of the ganglion, and supply the mucous membrane of the mouth and the duct of the submaxillary gland, some being lost in the submaxillary gland. The branch of communication from the lingual to the forepart of the ganglion is by some regarded as a branch of distribution, through which filaments pass from the ganglion to the lingual nerve, and by it are conveyed to the sublingual gland and the tongue. | 80 |
| |
| Trigeminal Nerve Reflexes.—Pains referred to various branches of the trigeminal nerve are of very frequent occurrence, and should always lead to a careful examination in order to discover a local cause. As a general rule the diffusion of pain over the various branches of the nerve is at first confined to one only of the main divisions, and the search for the causative lesion should always commence with a thorough examination of all those parts which are supplied by that division; although in severe cases pain may radiate over the branches of the other main divisions. The commonest example of this condition is the neuralgia which is so often associated with dental caries—here, although the tooth itself may not appear to be painful, the most distressing referred pains may be experienced, and these are at once relieved by treatment directed to the affected tooth. | 81 |
| Many other examples of trigeminal reflexes could be quoted, but it will be sufficient to mention the more common ones. Dealing with the ophthalmic nerve, severe supraorbital pain is commonly associated with acute glaucoma or with disease of the frontal or ethmoidal air cells. Malignant growths or empyema of the maxillary antrum, or unhealthy conditions about the inferior conchæ or the septum of the nose, are often found giving rise to “second division” neuralgia, and should be always looked for in the absence of dental disease in the maxilla. | 82 |
| It is on the mandibular nerve, however, that some of the most striking reflexes are seen. It is quite common to meet with patients who complain of pain in the ear, in whom there is no sign of aural disease, and the cause is usually to be found in a carious tooth in the mandible. Moreover, with an ulcer or cancer of the tongue, often the first pain to be experienced is one which radiates to the ear and temporal fossa, over the distribution of the auriculotemporal nerve. | 83 |