(Intestinum Tenue)
The small intestine is a convoluted tube, extending from the pylorus to the colic valve, where it ends in the large intestine. It is about 7 meters long, 168 and gradually diminishes in size from its commencement to its termination. It is contained in the central and lower part of the abdominal cavity, and is surrounded above and at the sides by the large intestine; a portion of it extends below the superior aperture of the pelvis and lies in front of the rectum. It is in relation, in front, with the greater omentum and abdominal parietes, and is connected to the vertebral column by a fold of peritoneum, the mesentery. The small intestine is divisible into three portions: the duodenum, the jejunum, and the ileum. | 1 |
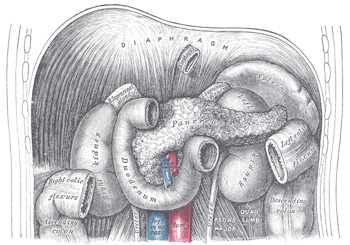 |
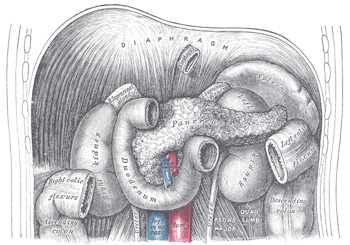
FIG. 1056– The duodenum and pancreas. (See enlarged image) |
| |
| The Duodenum (Fig. 1056) has received its name from being about equal in length to the breadth of twelve fingers (25 cm.). It is the shortest, the widest, and the most fixed part of the small intestine, and has no mesentery, being only partially covered by peritoneum. Its course presents a remarkable curve, somewhat of the shape of an imperfect circle, so that its termination is not far removed from its starting-point. | 2 |
| In the adult the course of the duodenum is as follows: commencing at the pylorus it passes backward, upward, and to the right, beneath the quadrate lobe of the liver to the neck of the gall-bladder, varying slightly in direction according to the degree of distension of the stomach: it then takes a sharp curve and descends along the right margin of the head of the pancreas, for a variable distance, generally to the level of the upper border of the body of the fourth lumbar vertebra. It now takes a second bend, and passes from right to left across the vertebral column, having a slight inclination upward; and on the left side of the vertebral column it ascends for about 2.5 cm., and then ends opposite the second lumbar vertebra in the jejunum. As it unites with the jejunum it turns abruptly forward, forming the duodendojejunal flexure. From the above description it will be seen that the duodenum may be divided into four portions: superior, descending, horizontal, and ascending. | 3 |
 |
FIG. 1057– Interior of the descending portion of the duodenum, showing bile papilla. (See enlarged image) |
| |
| |
| Relations.—The superior portion (pars superior; first portion) is about 5 cm. long. Beginning at the pylorus, it ends at the neck of the gall-bladder. It is the most movable of the four portions. It is almost completely covered by peritoneum, but a small part of its posterior surface near the neck of the gall-bladder and the inferior vena cava is uncovered; the upper border of its first half has the hepatoduodenal ligament attached to it, while to the lower border of the same segment the greater omentum is connected. It is in such close relation with the gall-bladder that it is usually found to be stained by bile after death, especially on its anterior surface. It is in relation above and in front with the quadrate lobe of the liver and the gall-bladder; behind with the gastroduodenal artery, the common bile duct, and the portal vein; and below and behind with the head and neck of the pancreas. | 4 |
| The descending portion (pars descendens; second portion) is from 7 to 10 cm. long, and extends from the neck of the gall-bladder, on a level with the first lumbar vertebra, along the right side of the vertebral column as low as the upper border of the body of the fourth lumbar vertebra. It is crossed in its middle third by the transverse colon, the posterior surface of which is uncovered by peritoneum and is connected to the duodenum by a small quantity of connective tissue. The supra- and infracolic portions are covered in front by peritoneum, the infracolic part by the right leaf of the mesentery. Posteriorly the descending portion of the duodenum is not covered by peritoneum. The descending portion is in relation, in front, from above downward, with the duodenal impression on the right lobe of the liver, the transverse colon, and the small intestine; behind, it has a variable relation to the front of the right kidney in the neighborhood of the hilum, and is connected to it by loose areolar tissue; the renal vessels, the inferior vena cava, and the Psoas below, are also behind it. At its medial side is the head of the pancreas, and the common bile duct; to its lateral side is the right colic flexure. The common bile duct and the pancreatic duct together perforate the medial side of this portion of the intestine obliquely (Figs. 1057 and 1100), some 7 to 10 cm. below the pylorus; the accessory pancreatic duct sometimes pierces it about 2 cm. above and slightly in front of these. | 5 |
| The horizontal portion (pars horizontalis; third or preaortic or transverse portion) is from 5 to 7.5 cm. long. It begins at the right side of the upper border of the fourth lumbar vertebra and passes from right to left, with a slight inclination upward, in front of the great vessels and crura of the diaphragm, and ends in the ascending portion in front of the abdominal aorta. It is crossed by the superior mesenteric vessels and the mesentery. Its front surface is covered by peritoneum, except near the middle line, where it is crossed by the superior mesenteric vessels. Its posterior surface is uncovered by peritoneum, except toward its left extremity, where the posterior layer of the mesentery may sometimes be found covering it to a variable extent. This surface rests upon the right crus of the diaphragm, the inferior vena cava, and the aorta. The upper surface is in relation with the head of the pancreas. | 6 |
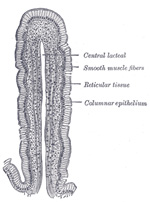
| The ascending portion (pars ascendens; fourth portion) of the duodenum is about 2.5 cm long. It ascends on the left side of the aorta, as far as the level of the upper border of the second lumbar vertebra, where it turns abruptly forward to become the jejunum, forming the duodenojejunal flexure. It lies in front of the left Psoas major and left renal vessels, and is covered in front, and partly at the sides, by peritoneum continuous with the left portion of the mesentery. | 7 |
| The superior part of the duodenum, as stated above, is somewhat movable, but the rest is practically fixed, and is bound down to neighboring viscera and the posterior abdominal wall by the peritoneum. In addition to this, the ascending part of the duodenum and the duodenojejunal flexure are fixed by a structure to which the name of Musculus suspensorius duodeni has been given. This structure commences in the connective tissue around the celiac artery and left crus of the diaphragm, and passes downward to be inserted into the superior border of the duodenojejunal curve and a part of the ascending duodenum, and from this it is continued into the mesentery. It possesses, according to Treitz, plain muscular fibers mixed with the fibrous tissue of which it is principally made up. It is of little importance as a muscle, but acts as a suspensory ligament. | 8 |
| |
| Vessels and Nerves.—The arteries supplying the duodenum are the right gastric and superior pancreaticoduodenal branches of the hepatic, and the inferior pancreaticoduodenal branch of the superior mesenteric. The veins end in the lienal and superior mesenteric. The nerves are derived from the cœliac plexus. | 9 |
| |
| Jejunum and Ileum.—The remainder of the small intestine from the end of the duodenum is named jejunum and ileum; the former term being given to the upper two-fifths and the latter to the lower three-fifths. There is no morphological line of distinction between the two, and the division is arbitrary; but at the same time the character of the intestine gradually undergoes a change from the commencement of the jejunum to the end of the ileum, so that a portion of the bowel taken from these two situations would present characteristic and marked differences. These are briefly as follows: | 10 |
| The Jejunum (intestinum jejunum) is wider, its diameter being about 4 cm., and is thicker, more vascular, and of a deeper color than the ileum, so that a given length weighs more. The circular folds (valvulæ conniventes) of its mucous membrane are large and thickly set, and its villi are larger than in the ileum. The aggregated lymph nodules are almost absent in the upper part of the jejunum, and in the lower part are less frequently found than in the ileum, and are smaller and tend to assume a circular form. By grasping the jejunum between the finger and thumb the circular folds can be felt through the walls of the gut; these being absent in the lower part of the ileum, it is possible in this way to distinguish the upper from the lower part of the small intestine. | 11 |
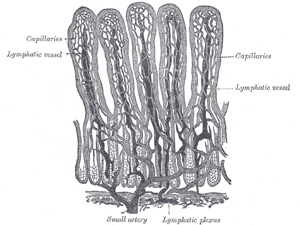
 |
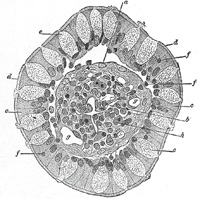
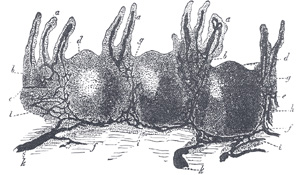
FIG. 1058– Section of duodenum of cat. (After Schäfer.) X 60. (See enlarged image) |
| |
| The Ileum (intestinum ileum) is narrow, its diameter being 3.75 cm., and its coats thinner and less vascular than those of the jejunum. It possesses but few circular folds, and they are small and disappear entirely toward its lower end, but aggregated lymph nodules (Peyer’s patches) are larger and more numerous. The jejunum for the most part occupies the umbilical and left iliac regions, while the ileum occupies chiefly the umbilical, hypogastric, right iliac, and pelvic regions. The terminal part of the ileum usually lies in the pelvis, from which it ascends over the right Psoas and right iliac vessels; it ends in the right iliac fossa by opening into the medial side of the commencement of the large intestine. The jejunum and ileum are attached to the posterior abdominal wall by an extensive fold of peritoneum, the mesentery, which allows the freest motion, so that each coil can accommodate itself to changes in form and position. The mesentery is fan-shaped; its posterior border or root, about 15 cm. long, is attached to the posterior abdominal wall from the left side of the body of the second lumbar vertebra to the right sacroiliac articulation, crossing successively the horizontal part of the duodenum, the aorta, the inferior vena cava, the ureter, and right Psoas muscle (Fig. 1040). Its breadth between its vertebral and intestinal borders averages about 20 cm., and is greater in the middle than at its upper and lower ends. According to Lockwood it tends to increase in breadth as age advances. Between the two layers of which it is composed are contained bloodvessels, nerves, lacteals, and lymph glands, together with a variable amount of fat. | 12 |
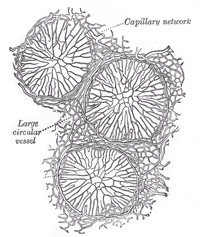
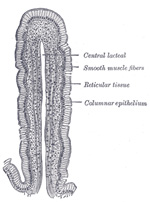 |
FIG. 1059– Vertical section of a villus from the dog’s small intestine. X 80. (See enlarged image) |
| |
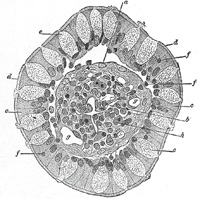 |
FIG. 1060– Transverse section of a villus, from the human intestine. (v. Ebner.) X 350. a. Basement membrane, here somewhat shrunken away from the epithelium. b. Lacteal. c. Columnar epithelium. d. Its striated border. e. Goblet cells. f. Leucocytes in epithelium. f’. Leucocytes below epithelium. g. Bloodvessels. h. Muscle cells cut across. (See enlarged image) |
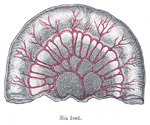
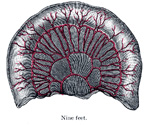
| |
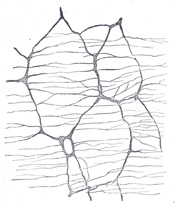
| |
| Meckel’s Diverticulum (diverticulum ilei).—This consists of a pouch which projects from the lower part of the ileum in about 2 per cent. of subjects. Its average position is about 1 meter above the colic valve, and its average length about 5 cm. Its caliber is generally similar to that of the ileum, and its blind extremity may be free or may be connected with the abdominal wall or with some other portion of the intestine by a fibrous band. It represents the remains of the proximal part of the vitelline duct, the duct of communication between the yolk-sac and the primitive digestive tube in early fetal life. | 13 |
| |
| Structure.—The wall of the small intestine (Fig. 1058) is composed of four coats: serous, muscular, areolar, and mucous. | 14 |
| The serous coat (tunica serosa) is derived from the peritoneum. The superior portion of the duodenum is almost completely surrounded by this membrane near its pyloric end, but is only covered in front at the other extremity; the descending portion is covered by it in front, except where it is carried off by the transverse colon; and the inferior portion lies behind the peritoneum which passes over it without being closely incorporated with the other coats of this part of the intestine, and is separated from it in and near the middle line by the superior mesenteric vessels. The rest of the small intestine is surrounded by the peritoneum, excepting along its attached or mesenteric border; here a space is left for the vessels and nerves to pass to the gut. | 15 |
| The muscular coat (tunica muscularis) consists of two layers of unstriped fibers: an external, longitudinal, and an internal, circular layer. The longitudinal fibers are thinly scattered over the surface of the intestine, and are more distinct along its free border. The circular fibers form a thick, uniform layer, and are composed of plain muscle cells of considerable length. The muscular coat is thicker at the upper than at the lower part of the small intestine. | 16 |
| The areolar or submucous coat (tela submucosa) connects together the mucous and muscular layers. It consists of loose, filamentous areolar tissue containing bloodvessels, lymphatics, and nerves. It is the strongest layer of the intestine. | 17 |
| The mucous membrane (tunica mucosa) is thick and highly vascular at the upper part of the small intestine, but somewhat paler and thinner below. It consists of the following structures: next the areolar or submucous coat is a double layer of unstriped muscular fibers, outer longitudinal and inner circular, the muscularis mucosæ internal to this is a quantity of retiform tissue, enclosing in its meshes lymph corpuscles, and in this the bloodvessels and nerves ramify; lastly, a basement membrane, supporting a single layer of epithelial cells, which throughout the intestine are columnar in character. The cells are granular in appearance, and each possesses a clear oval nucleus. At their superficial or unattached ends they present a distinct layer of highly refracting material, marked by vertical striæ, the striated border. | 18 |
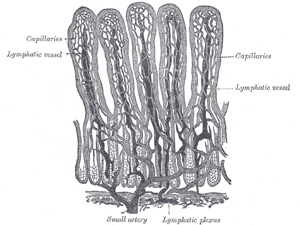 |
FIG. 1061– Villi of small intestine, showing bloodvessels and lymphatic vessels. (Cadiat.) (See enlarged image) |
| |
| The mucous membrane presents for examination the following structures, contained within it or belonging to it: | 19 |
| Circular folds. |
| Duodenal glands. |
| Villi. |
| Solitary lymphatic nodules. |
| Intestinal glands. |
| Aggregated lymphatic nodules. |
|
 |
FIG. 1062– An intestinal gland from the human intestine. (Flemming.) (See enlarged image) |
| |
| The circular folds (plicæ circulares [Kerkringi]; valvulæ conniventes; valves of Kerkring) are large valvular flaps projecting into the lumen of the bowel. They are composed of reduplications of the mucous membrane, the two layers of the fold being bound together by submucous tissue; unlike the folds in the stomach, they are permanent, and are not obliterated when the intestine is distended. The majority extend transversely around the cylinder of the intestine for about one-half or two-thirds of its circumference, but some form complete circles, and others have a spiral direction; the latter usually extend a little more than once around the bowel, but occasionally two or three times. The larger folds are about 8 mm. in depth at their broadest part; but the greater number are of smaller size. The larger and smaller folds alternate with each other. They are not found at the commencement of the duodenum, but begin to appear about 2.5 or 5 cm. beyond the pylorus. In the lower part of the descending portion, below the point where the bile and pancreatic ducts enter the intestine, they are very large and closely approximated. In the horizontal and ascending portions of the duodenum and upper half of the jejunum they are large and numerous, but from this point, down to the middle of the ileum, they diminish considerably in size. In the lower part of the ileum they almost entirely disappear; hence the comparative thinness of this portion of the intestine, as compared with the duodenum and jejunum. The circular folds retard the passage of the food along the intestines, and afford an increased surface for absorption. | 20 |
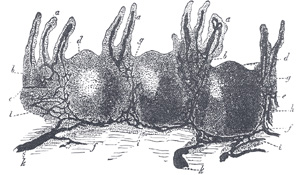 |
FIG. 1063– Vertical section of a human aggregated lymphatic nodule, injected through its lymphatic canals. a. Villi with their chyle passages. b. Intestinal glands. c. Muscularis mucosæ. d. Cupola or apex of solitary nodule. e. Mesial zone of nodule. f. Base of nodule. g. Points of exit of the lacteals from the villi, and entrance into the true mucous membrane. h. Retiform arrangement of the lymphatics in the mesial zone. i. Course of the latter at the base of the nodule. k. Confluence of the lymphatics opening into the vessels of the submucous tissue. l. Follicular tissue of the latter. (See enlarged image) |
| |
| The intestinal villi (villi intestinales) are highly vascular processes, projecting from the mucous membrane of the small intestine throughout its whole extent, and giving to its surface a velvety appearance. They are largest and most numerous in the duodenum and jejunum, and become fewer and smaller in the ileum. | 21 |
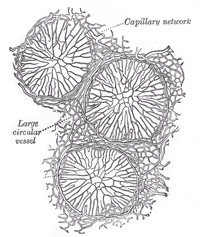 |
FIG. 1064– Transverse section through the equatorial plane of three aggregated lymphatic nodules from the rabbit. (See enlarged image) |
| |
| Structure of the villi (Figs. 1059, 1060).—The essential parts of a villus are: the lacteal vessel, the bloodvessels, the epithelium, the basement membrane, and the muscular tissue of the mucosa, all being supported and held together by retiform lymphoid tissue. | 22 |
| The lacteals are in some cases double, and in some animals multiple, but usually there is a single vessel. Situated in the axis of the villus, each commences by dilated cecal extremities near to, but not quite at, the summit of the villus. The walls are composed of a single layer of endothelial cells. | 23 |
| The muscular fibers are derived from the muscularis mucosæ, and are arranged in longitudinal bundless around the lacteal vessel, extending from the base to the summit of the villus, and giving off, laterally, individual muscle cells, which are enclosed by the reticulum, and by it are attached to the basement-membrane and to the lacteal. | 24 |
| The bloodvessels (Fig. 1061) form a plexus under the basement membrane, and are enclosed in the reticular tissue. | 25 |
| These structures are surrounded by the basement membrane, which is made up of a stratum of endothelial cells, and upon this is placed a layer of columnar epithelium, the characteristics of which have been described. The retiform tissue forms a net-work (Fig. 1060) in the meshes of which a number of leucocytes are found. | 26 |
 |
FIG. 1065– No caption. (See enlarged image) |
| |
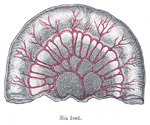 |
FIG. 1066– No caption. (See enlarged image) |
| |
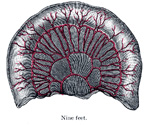 |
FIG. 1067– No caption. (See enlarged image) |
| |
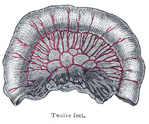 |
FIG. 1068– No caption. (See enlarged image) |
| |
 |
FIG. 1069– No caption. (See enlarged image) |
| |
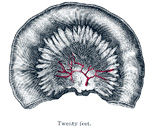 |
FIG. 1070– —Diagrams showing the arrangement and variations of the loops of the mesenteric vessels for various segments of the small intestine of average length. Nearest the duodenum the mesenteric loops are primary, the vasa recta are long and regular in distribution, and the translucent spaces (lunettes) are extensive. Toward the ileocolic junction, secondary and tertiary loops are observed, the vessels are smaller and become obscured by numerous fat-tabs. (After Monks.) (See enlarged image) |
| |
| The intestinal glands (glandulæ intestinales [Lieberkühni]; crypts of Lieberkühn) (Fig. 1062) are found in considerable numbers over every part of the mucous membrane of the small intestine. They consist of minute tubular depressions of the mucous membrane, arranged perpendicularly to the surface, upon which they open by small circular apertures. They may be seen with the aid of a lens, their orifices appearing as minute dots scattered between the villi. Their walls are thin, consisting of a basement membrane lined by columnar epithelium, and covered on their exterior by capillary vessels. | 27 |
| The duodenal glands (glandulæ duodenales [Brunneri]; Brunner’s glands) are limited to the duodenum (Fig. 1058), and are found in the submucous areolar tissue. They are largest and most numerous near the pylorus, forming an almost complete layer in the superior portion and upper half of the descending portions of the duodenum. They then begin to diminish in number, and practically disappear at the junction of the duodenum and jejunum. They are small compound acinotubular glands consisting of a number of alveoli lined by short columnar epithelium and opening by a single duct on the inner surface of the intestine. | 28 |
| The solitary lymphatic nodules (noduli lymphatici solitarii; solitary glands) are found scattered throughout the mucous membrane of the small intestine, but are most numerous in the lower part of the ileum. Their free surfaces are covered with rudimentary villi, except at the summits, and each gland is surrounded by the openings of the intestinal glands. Each consists of a dense interlacing retiform tissue closely packed with lymph-corpuscles, and permeated with an abundant capillary network. The interspaces of the retiform tissue are continuous with larger lymph spaces which surround the gland, through which they communicate with the lacteal system. They are situated partly in the submucous tissue, partly in the mucous membrane, where they form slight projections of its epithelial layer (see Fig. 1082). | 29 |
| The aggregated lymphatic nodules (noduli lymphatici aggregati; Peyer’s patches; Peyer’s glands; agminated follicles; tonsillæ intestinales) (Fig. 1063) form circular or oval patches, from twenty to thirty in number, and varying in length from 2 to 10 cm. They are largest and most numerous in the ileum. In the lower part of the jejunum they are small, circular, and few in number. They are occasionally seen in the duodenum. They are placed lengthwise in the intestine, and are situated in the portion of the tube most distant from the attachment of the mesentery. Each patch is formed of a group of solitary lymphatic nodules covered with mucous membrane, but the patches do not, as a rule, possess villi on their free surfaces. They are best marked in the young subject, become indistinct in middle age, and sometimes disappear altogether in advanced life. They are freely supplied with bloodvessels (Fig. 1064), which form an abundant plexus around each follicle and give off fine branches permeating the lymphoid tissue in the interior of the follicle. The lymphatic plexuses are especially abundant around these patches. | 30 |
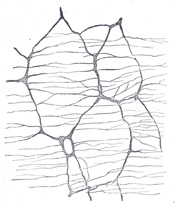 |
FIG. 1071– The myenteric plexus from the rabbit. X 50. (See enlarged image) |
| |
 |
FIG. 1072– The plexus of the submucosa from the rabbit. X 50. (See enlarged image) |
| |
| |
| Vessels and Nerves.—The jejunum and ileum are supplied by the superior mesenteric artery, the intestinal branches of which, having reached the attached border of the bowel, run between the serous and muscular coats, with frequent inosculations to the free border, where they also anastomose with other branches running around the opposite surface of the gut. From these vessels numerous branches are given off, which pierce the muscular coat, supplying it and forming an intricate plexus in the submucous tissue. From this plexus minute vessels pass to the glands and villi of the mucous membrane. The veins have a similar course and arrangement to the arteries. The lymphatics of the small intestine (lacteals) are arranged in two sets, those of the mucous membrane and those of the muscular coat. The lymphatics of the villi commence in these structures in the manner described above. They form an intricate plexus in the mucous and submucous tissue, being joined by the lymphatics from the lymph spaces at the bases of the solitary nodules, and from this pass to larger vessels at the mesenteric border of the gut. The lymphatics of the muscular coat are situated to a great extent between the two layers of muscular fibers, where they form a close plexus; throughout their course they communicate freely with the lymphatics from the mucous membrane, and empty themselves in the same manner as these into the origins of the lacteal vessels at the attached border of the gut. | 31 |
| The nerves of the small intestines are derived from the plexuses of sympathetic nerves around the superior mesenteric artery. From this source they run to the myenteric plexus (Auerbach’s plexus) (Fig. 1071) of nerves and ganglia situated between the circular and longitudinal muscular fibers from which the nervous branches are distributed to the muscular coats of the intestine. From this a secondary plexus, the plexus of the submucosa (Meissner’s plexus) (Fig. 1072) is derived, and is formed by branches which have perforated the circular muscular fibers. This plexus lies in the submucous coat of the intestine; it also contains ganglia from which nerve fibers pass to the muscularis mucosæ and to the mucous membrane. The nerve bundles of the submucous plexus are finer than those of the myenteric plexus. | 32 |